Page 100 - GHES-2-1
P. 100
Global Health Econ Sustain Transgenders HIV-related knowledge and risk behaviors
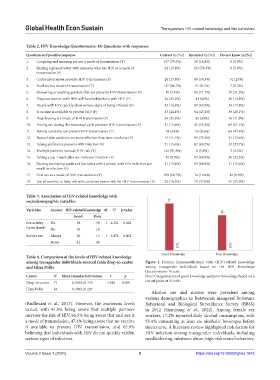
Table 2. HIV Knowledge Questionnaire‑18: Questions with responses
Question and positive response Correct (n [%]) Incorrect (n [%]) Do not know (n [%])
1. Coughing and sneezing are not a mode of transmission (T) 107 (79.3%) 20 (14.8%) 8 (5.9%)
2. Sharing a glass of water with someone who has HIV as a mode of 24 (17.8%) 103 (76.3%) 8 (5.9%)
transmission (F)
3. Coitus interruptus prevents HIV transmission (F) 24 (17.8%) 80 (59.3%) 31 (23%)
4. Anal sex is a mode of transmission (T) 117 (86.7%) 11 (8.1%) 7 (5.2%)
5. Showering or washing genitals after sex prevents HIV transmission (F) 10 (7.4%) 96 (71.1%) 29 (21.5%)
6. Pregnant women with HIV will have babies born with HIV (F) 34 (25.2%) 81 (60%) 20 (14.8%)
7. People with HIV quickly show serious signs of being infected (F) 22 (16.3%) 89 (65.9%) 24 (17.8%)
8. A vaccine is available to prevent HIV (F) 33 (24.4%) 64 (47.4%) 38 (28.1%)
9. Deep kissing is a mode of HIV transmission (F) 34 (25.2%) 85 (63%) 16 (11.9%)
10. Having sex during the menstrual cycle prevents HIV transmission (F) 21 (15.6%) 45 (33.3%) 69 (51.1%)
11. Female condoms can prevent HIV transmission (T) 58 (43%) 13 (9.6%) 64 (47.4%)
12. Natural skin condoms are more effective than latex condoms (F) 15 (11.1%) 99 (73.3%) 21 (15.6%)
13. Taking antibiotics prevents HIV infection (F) 21 (15.6%) 82 (60.7%) 32 (23.7%)
14. Multiple partners increase HIV risk (T) 124 (91.9%) 8 (5.9%) 3 (2.2%)
15. Taking a test 1 week after sex indicates infection (F) 12 (8.9%) 93 (68.9%) 30 (22.2%)
16. Sharing swimming pools and hot tubes with a person with HIV infection can 21 (15.6%) 93 (68.9%) 21 (15.6%)
result in infection (F)
17. Oral sex as a mode of HIV transmission (T) 109 (80.7%) 14 (10.4%) 12 (8.9%)
18. Use of vaseline or baby oils with condoms lowers risk for HIV transmission (F) 22 (16.3%) 78 (57.8%) 35 (25.9%)
Table 3. Association of HIV‑related knowledge with
sociodemographic variables 77
Variables Answer HIV‑related Knowledge df Χ 2 p‑value
58
Good Poor
Sex activity Yes 38 39 1 4.321 0.028
(open street) No 39 19
Barrier use Always 36 13 1 8.476 0.003
Never 41 45
57% 43%
Good Knowledge Poor Knowledge
Table 4. Comparison of the levels of HIV‑related knowledge
among transgender individuals sourced from drop‑in‑center Figure 1. Human immunodeficiency virus (HIV)-related knowledge
and Hijra Pollis among transgender individuals based on the HIV Knowledge
Questionnaire-18 scale.
Center N Mean±standard deviation t p Note: Categorization of good knowledge and poor knowledge based on a
Drop-in-center 71 0.5548±0.176 4.816 0.000 cut-off point of 47.44%.
Hijra Pollis 64 0.3863±0.224
Alcohol use and misuse were prevalent among
various demographics in Botswana’s inaugural Botswana
(Budhwani et al., 2017). However, the awareness levels Behavioral and Biological Surveillance Survey (BBSS)
varied, with 91.9% being aware that multiple partners in 2012 (Siamisang et al., 2022). Among female sex
increase the risk of HIV, 86.5% being aware that anal sex is workers, 17.2% reported daily alcohol consumption, with
a mode of transmission, 47.4% being aware that no vaccine 55.4% consuming at least six alcoholic beverages before
is available to prevent HIV transmission, and 65.9% intercourse. A literature review highlighted risk factors for
believing that individuals with HIV do not quickly exhibit HIV infection among transgender individuals, including
serious signs of infection. needle sharing, substance abuse, high-risk sexual behaviors,
Volume 2 Issue 1 (2024) 5 https://doi.org/10.36922/ghes.1643