Page 31 - ITPS-7-1
P. 31
INNOSC Theranostics and
Pharmacological Sciences Antiplatelet treatments in neurological patients
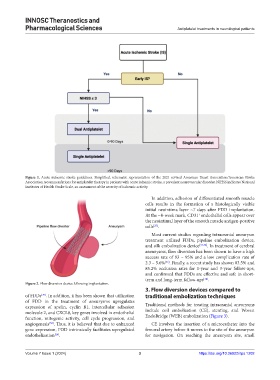
Figure 1. Acute ischemic stroke guidelines. Simplified, schematic representation of the 2021 revised American Heart Association/American Stroke
Association recommendations for antiplatelet therapy in patients with acute ischemic stroke, a prevalent neurovascular disorder. NIHSS indicates National
Institutes of Health Stroke Scale, an assessment of the severity of ischemic activity.
In addition, adhesion of differentiated smooth muscle
cells results in the formation of a histologically visible
initial neointima layer ~7 days after FDD implantation.
At the ~8-week mark, CD31 endothelial cells appear over
+
the neointimal layer of the smooth muscle antigen-positive
cells .
[27]
Most current studies regarding intracranial aneurysm
treatment utilized FDDs, pipeline embolization device,
and silk embolization device [31,32] . In treatment of cerebral
aneurysms, flow diversion has been shown to have a high
success rate of 93 – 95% and a low complication rate of
2.3 – 5.6% . Finally, a recent study has shown 83.5% and
[33]
85.2% occlusion rates for 1-year and 3-year follow-ups,
and confirmed that FDDs are effective and safe in short-
term and long-term follow-ups .
[34]
Figure 2. Flow diversion device following implantation.
3. Flow diversion devices compared to
of FDDs . In addition, it has been shown that utilization traditional embolization techniques
[29]
of FDD in the treatment of aneurysms upregulates
expression of apelin, cyclin B1, intercellular adhesion Traditional methods for treating intracranial aneurysms
molecule 2, and CXCL8, key genes involved in endothelial include coil embolization (CE), stenting, and Woven
function, mitogenic activity, cell cycle progression, and EndoBridge (WEB) embolization (Figure 3).
angiogenesis . Thus, it is believed that due to enhanced CE involves the insertion of a microcatheter into the
[30]
gene expression, FDD intrinsically facilitates upregulated femoral artery before it moves to the site of the aneurysm
endothelization . for navigation. On reaching the aneurysm site, small
[26]
Volume 7 Issue 1 (2024) 3 https://doi.org/10.36922/itps.1202