Page 60 - AN-1-3
P. 60
Advanced Neurology Targets and medications for AVM of CNS
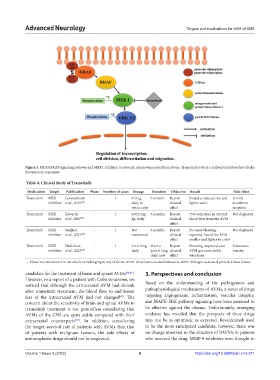
Figure 1. KRAS/BRAF signaling pathway and MEK1 inhibitor in sporadic arteriovenous malformations. Trametinib acts as a pathway inhibitor that blocks
downstream responses.
Table 4. Clinical Study of Trametinib.
Medication Target Publication Phase Number of cases Dosage Duration Objective Result Side effect
Trametinib MEK Lekwuttikarn - 1 0.5mg, 6 months Report Found a reduced size and A mild
inhibitor et al., 2019 [63] daily to clinical lighter color acneiform
twice a day effect eruption
Trametinib MEK Edwards - 1 0.025 mg/ 6 months Report 75% reduction in arterial Not displayed
inhibitor et al. 2020 [61] kg, daily clinical blood flow from the AVM
effect
Trametinib MEK Samkari - 1 Not 6 months Report No more bleeding Not displayed
inhibitor et al., 2021 [64] mentioned clinical reported, found the AVM
effect smaller and lighter in color
Trametinib MEK Nicholson - 1 2.0-0.5mg, Over a Report Shunting improved and Cutaneous
inhibitor et al., 2022 [62] daily year, 0.5mg clinical AVM got more stable toxicity
daily now effect structures
–: Phase not mentioned in the article or belonging to any of them, AVM: Arteriovenous malformation, MEK: Mitogen-activated protein kinase kinase
candidate for the treatment of brain and spinal AVMs [60,66] . 3. Perspectives and conclusion
However, in a report of a patient with Cobb syndrome, we
noticed that although the extracranial AVM had shrunk Based on the understanding of the pathogenesis and
after trametinib treatment, the blood flow to and lesion pathophysiological mechanisms of AVMs, a series of drugs
size of the intracranial AVM had not changed . The targeting angiogenesis, inflammation, vascular integrity,
[61]
concern about the sensitivity of brain and spinal AVMs to and MAPK-ERK pathway signaling have been assumed to
trametinib treatment is not groundless considering that be effective against the disease. Unfortunately, emerging
AVMs of the CNS are quite stable compared with their evidence has revealed that the prospects of these drugs
extracranial counterparts . In addition, considering may not be as optimistic as expected. Bevacizumab used
[67]
the longer survival rate of patients with AVMs than that to be the most anticipated candidate; however, there was
of patients with malignant tumors, the side effects of no change observed in the structure of BAVMs in patients
antineoplastic drugs should not be neglected. who received the drug. MMP-9 inhibitors were thought to
Volume 1 Issue 3 (2022) 6 https://doi.org/10.36922/an.v1i3.211