Page 194 - EJMO-9-2
P. 194
Eurasian Journal of
Medicine and Oncology Prevalence of PPD in Baghdad
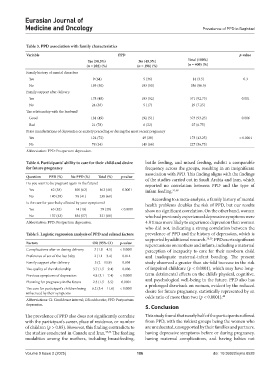
Table 3. PPD association with family characteristics
Variable PPD p-value
Yes (50.5%) No (49.5%) Total (100%)
(n = 202) (%) (n = 198) (%) (n = 400) (%)
Family history of mental disorders
Yes 9 (64) 5 (36) 14 (3.5) 0.3
No 193 (50) 193 (50) 386 (96.5)
Family support after delivery
Yes 178 (48) 193 (52) 371 (92.75) 0.001
No 24 (83) 5 (17) 29 (7.25)
The relationship with the husband
Good 181 (49) 192 (51) 373 (93.25) 0.006
Bad 21 (78) 6 (22) 27 (6.75)
Prior manifestations of depression or anxiety preceding or during the most recent pregnancy
Yes 124 (72) 49 (28) 173 (43.25) < 0.0001
No 78 (34) 149 (66) 227 (56.75)
Abbreviation: PPD: Postpartum depression.
Table 4. Participants’ ability to care for their child and desire bottle feeding, and mixed feeding, exhibit a comparable
for future pregnancy frequency across the groups, resulting in an insignificant
association with PPD. This finding aligns with the findings
Question PPD (%) No PPD (%) Total (%) p-value of the studies carried out in Saudi Arabia and Iran, which
Do you want to be pregnant again in the future? reported no correlation between PPD and the type of
Yes 62 (38) 100 (62) 162 (40) 0.0001 infant feeding. 37,38
No 140 (59) 98 (41) 238 (60) According to a meta-analysis, a family history of mental
Is the care for your baby affected by your symptoms? health problems doubles the risk of PPD, but our results
Yes 65 (82) 14 (18) 79 (20) < 0.0001 show no significant correlation. On the other hand, women
No 137 (43) 184 (57) 321 (80) who had previously experienced depressive symptoms were
Abbreviation: PPD: Postpartum depression. 4.8 times more likely to experience depression than women
who did not, indicating a strong correlation between the
Table 5. Logistic regression analysis of PPD and related factors prevalence of PPD and the history of depression, which is
supported by additional research. 38,39 . PPD exerts significant
Factors OR (95% CI) p-value repercussions on mothers and infants, including a maternal
Complications after or during delivery 3 (1.8 – 4.5) < 0.0001 perception of incapacity to care for their newborn child
Preference of sex of the last baby 2 (1.1 – 3.4) 0.014 and inadequate maternal-infant bonding. The present
Family support after delivery 5 (2 – 13.9) 0.001 study observed a greater than six-fold increase in the risk
The quality of the relationship 3.7 (1.5 – 9.4) 0.006 of impaired childcare (p < 0.0001), which may have long-
Previous symptoms of depression 4.8 (3.1 – 7.4) < 0.0001 term detrimental effects on the child’s physical, cognitive,
Planning for pregnancy in the future 2.3 (1.5 – 3.5) 0.0001 and psychological well-being in the future. PPD also has
a prolonged drawback on women, evident by the reduced
The care for participant’s children being 6.2 (3.4 – 11.6) < 0.0001 desire for future pregnancy, statistically represented by an
influenced by their symptoms
odds ratio of more than two (p < 0.0001). 40
Abbreviations: CI: Confidence interval; OR: odds ratio; PPD: Postpartum
depression.
5. Conclusion
The prevalence of PPD also does not significantly correlate This study found that nearly half of the participants suffered
with the participant’s career, place of residence, or number from PPD, with the riskiest groups being the women who
of children (p > 0.05). However, this finding contradicts to are uneducated, unsupported by their families and partners,
the studies conducted in Canada and Iran. 35,36 The feeding having depressive symptoms before or during pregnancy,
modalities among the mothers, including breastfeeding, having maternal complications, and having babies not
Volume 9 Issue 2 (2025) 186 doi: 10.36922/ejmo.8528