Page 25 - ESAM-1-4
P. 25
Engineering Science in
Additive Manufacturing Machine learning for biomedical metal AM
A B
C
D E
11
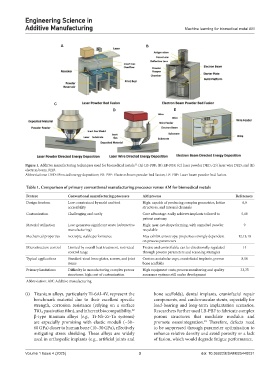
Figure 1. Additive manufacturing techniques used for biomedical metals. (A) LB-PBF; (B) EB-PBF; (C) laser powder DED; (D) laser wire DED; and (E)
electron beam DED.
Abbreviations: DED: Directed energy deposition; EB-PBF: Electron beam powder bed fusion; LB-PBF: Laser beam powder bed fusion.
Table 1. Comparison of primary conventional manufacturing processes versus AM for biomedical metals
Feature Conventional manufacturing processes AM process References
Design freedom Low: constrained by mold and tool High: capable of producing complex geometries, lattice 6,9
accessibility structures, and internal channels
Customization Challenging and costly Core advantage: easily achieves implants tailored to 5,10
patient anatomy
Material utilization Low: generates significant waste (subtractive High: near-net-shape forming, with unmelted powder 9
manufacturing) recyclable
Mechanical properties Isotropic, stable performance May exhibit anisotropy; properties strongly dependent 12,13,18
on process parameters
Microstructure control Limited by overall heat treatment, restricted Precise and controllable; can be directionally regulated 14
control range through process parameters and scanning strategies
Typical applications Standard-sized bone plates, screws, and joint Custom acetabular cups, craniofacial implants, porous 8,10
stems bone scaffolds
Primary limitations Difficulty in manufacturing complex porous High equipment costs; process monitoring and quality 33,35
structures; high cost of customization assurance systems still under development
Abbreviation: AM: Additive manufacturing.
(i) Titanium alloys, particularly Ti-6Al-4V, represent the bone scaffolds), dental implants, craniofacial repair
benchmark material due to their excellent specific components, and cardiovascular stents, especially for
strength, corrosion resistance (relying on a surface load-bearing and long-term implantation scenarios.
TiO₂ passivation film), and inherent biocompatibility. Researchers further used LB-PBF to fabricate complex
22
β-type titanium alloys (e.g., Ti-Nb-Zr-Ta systems) porous structures that modulate modulus and
are especially promising with elastic moduli (~30– promote osseointegration. Therefore, defects need
23
60 GPa) closer to human bone (10–30 GPa), effectively to be suppressed through parameter optimization to
mitigating stress shielding. These alloys are widely enhance relative density and avoid porosity or a lack
used in orthopedic implants (e.g., artificial joints and of fusion, which would degrade fatigue performance.
Volume 1 Issue 4 (2025) 3 doi: 10.36922/ESAM025440031