Page 77 - GTM-2-3
P. 77
Global Translational Medicine Thromboembolism risk in non-small-cell lung cancer
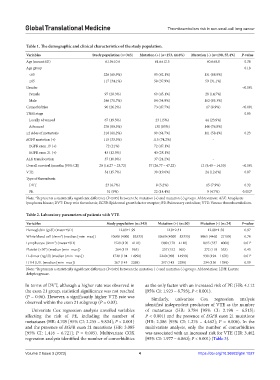
Table 1. The demographic and clinical characteristics of the study population.
Variables Study population (n=343) Mutation (+) (n=153, 44.6%) Mutation (‑) (n=190, 55.4%) P‑value
Age (mean±SD) 61.9±10.6 61.6±12.5 60.6±8.8 0.38
Age group 0.18
<65 226 (65.9%) 95 (62.1%) 131 (68.9%)
≥65 117 (34.1%) 58 (37.9%) 59 (31.1%)
Gender <0.001
Female 97 (28.3%) 69 (45.1%) 28 (14.7%)
Male 246 (71.7%) 84 (54.9%) 162 (85.3%)
Comorbidities 90 (26.2%) 73 (47.7%) 17 (8.9%) <0.001
TNM stage 0.05
Locally advanced 67 (19.5%) 23 (15%) 44 (23.9%)
Advanced 276 (80.5%) 130 (85%) 146 (76.8%)
≥2 sides of metastasis 210 (61.2%) 99 (64.7%) 111 (58.4%) 0.23
EGFR mutation (+) 115 (33.5%) 115 (74.2%) -
EGFR exon 19 (+) 72 (21%) 72 (47.1%)
EGFR exon 21 (+) 43 (12.5%) 43 (28.1%)
ALK translocation 37 (10.8%) 37 (24.2%) -
Overall survival (months [95% Cl]) 20 (16.27 – 23.72) 37 (26.77 – 47.22) 12 (9.49 – 14.50) <0.001
VTE 54 (15.7%) 30 (19.6%) 24 (12.6%) 0.07
Type of thrombosis
DVT 23 (6.7%) 8 (5.2%) 15 (7.9%) 0.32
PE 31 (9%) 22 (14.4%) 9 (4.7%) 0.002*
Note: *Represents a statistically significant difference (P<0.05) between the mutation (+) and mutation (-) groups. Abbreviation: ALK: Anaplastic
lymphoma kinase; DVT: Deep vein thrombosis; EGFR: Epidermal growth factor receptor; PE: Pulmonary embolism; VTE: Venous thromboembolism.
Table 2. Laboratory parameters of patients with VTE
Variables Study population (n=343) Mutation (+) (n=30) Mutation (‑) (n=24) P‑value
Hemoglobin (g/dl) (mean±SD) 12.89±1.99 12.9±2.31 12.88±1.58 0.97
White blood cell (/mm ) (median [min–max]) 10600 (4000 – 83333) 10600 (4000 – 83333) 9965 (4460 – 27100) 0.76
3
Lymphocyte (/mm ) (mean±SD) 1520 (170 – 4110) 1380 (170 – 4110) 1895 (537 – 4000) 0.01*
3
3
Platelet (×10 ) (median [min–max]) 264 (119 – 965) 257 (152 – 965) 272 (119 – 553) 0.45
D-dimer (ng/dl) (median [min–max]) 1720 (194 – 14990) 2240 (908 – 14990) 930 (194 – 1670) 0.01*
LDH (U/L (median [min–max]) 267 (143 – 2298) 297 (143 – 2298) 234 (156 – 1389) 0.09
Note: *Represents a statistically significant difference (P<0.05) between the mutation (+) and mutation (-) groups. Abbreviation: LDH: Lactate
dehydrogenase.
In terms of DVT, although a higher rate was observed in as the only factor with an increased risk of PE (HR: 4.112
the exon 21 group, statistical significance was not reached [95% CI: 1.923 – 8.793]; P < 0.001).
(P = 0.06). However, a significantly higher VTE rate was Similarly, univariate Cox regression analysis
observed within the exon 21 subgroup (P = 0.03). identified independent predictors of VTE as the number
Univariate Cox regression analysis unveiled variables of metastases (HR: 3.784 [95% CI: 2.198 – 6.515];
affecting the risk of PE, including the number of P < 0.001) and the presence of EGFR exon 21 mutations
metastases (HR: 4.709 [95% CI: 2.255 – 9.834]; P < 0.001) (HR: 2.386 [95% CI: 1.276 – 4.462]; P = 0.006). In the
and the presence of EGFR exon 21 mutations (HR: 3.085 multivariate analysis, only the number of comorbidities
[95% CI: 1.416 – 6.721]; P = 0.005). Multivariate COX was associated with an increased risk for VTE (HR: 3.462
regression analysis identified the number of comorbidities [95% CI: 1.977 – 6.060]; P < 0.001) (Table 3).
Volume 2 Issue 3 (2023) 4 https://doi.org/10.36922/gtm.1027