Page 49 - GTM-3-2
P. 49
Global Translational Medicine Prognostic indicators and management of SAP
Table 7. Principles of surgical management of acute pancreatitis
Atlanta Classification Therapeutic principles
Mild acute pancreatitis (edematous pancreatitis) • No surgery other than cholecystectomy during the same hospital stay
Severe acute pancreatitis
Sterile necrosis • No systematic surgery
• Surgery is indicated if there is no response to intensive care (when necrosis
exceeds half the pancreatic area), ductal interruption syndrome, recurrent
pancreatitis, or refeeding one
Infected necrosis • Mini‑invasive surgical debridement (VARD) + continuous lavage (step‑up
approach) or open packing (pancreaticostomy chimney) in the event of failure
(step-down approach)
Pancreatic abscess • Echo or scan‑guided drainage
• Surgical drainage in cases of persistent sepsis
Acute pseudocyst • Drainage by interventional radiology or surgery depends on the resources
available to the hospital center
Abbreviation: VARD: Video‑assisted retroperitoneal drainage.
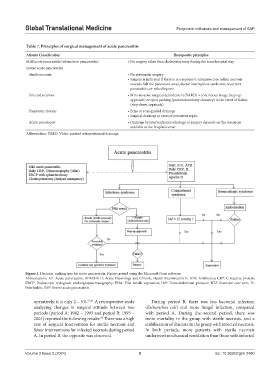
Figure 1. Decision‑making tree for acute pancreatitis. Figure created using the Microsoft Paint software.
Abbreviations: AP: Acute pancreatitis; APACHE II: Acute Physiology and Chronic Health Examination II; ATB: Antibiotics; CRP: C-reactive protein;
ERCP: Endoscopic retrograde cholangiopancreatography; FNA: Fine needle aspiration; IAP: Intra-abdominal pressure; ICU: Intensive care unit; IL:
Interleukin; SAP: Severe acute pancreatitis.
operatively, it is only 2 – 5%. 51,81 A retrospective study During period B, there was less bacterial infection
analyzing changes in surgical attitude between two (Escherichia coli) and more fungal infection, compared
periods (period A: 1982 – 1993 and period B: 1993 – with period A. During the second period, there was
2001) reported the following results: There was a high more mortality in the group with sterile necrosis, and a
82
rate of surgical intervention for sterile necrosis and stabilization of this rate in the group with infected necrosis.
fewer interventions for infected necrosis during period In both periods, more patients with sterile necrosis
A. In period B, the opposite was observed. underwent mechanical ventilation than those with infected
Volume 3 Issue 2 (2024) 8 doi: 10.36922/gtm.2480