Page 106 - GTM-4-3
P. 106
Global Translational Medicine Comparative analysis of MIF and CF techniques
(iii) Individuals who were pregnant or lactating.
(iv) Individuals who did not have baseline and/or
follow-up complete periodontal charts or clinical
notes, especially those not specifying the flap
technique used for PR.
2.2.3. Flap technique description
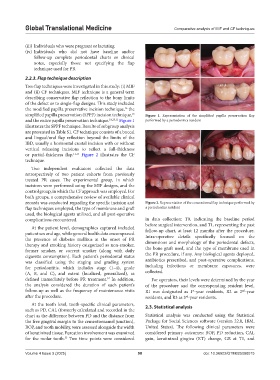
Two flap techniques were investigated in this study: (i) MIF
and (ii) CF techniques. MIF technique is a general term
describing conservative flap reflection to the bony limits
of the defect or to single-flap designs. This study included
the modified papilla preservative incision technique, the
16
simplified papilla preservation (SPPF) incision technique, Figure 1. Representation of the simplified papilla preservation flap
15
and the entire papilla preservation technique. 18,25,31 Figure 1 performed by a periodontics resident
illustrates the SPPF technique. Results of subgroup analysis
are presented in Table S1. CF technique consists of a buccal
and lingual/oral flap reflection beyond the limits of the
IBD, usually a horizontal crestal incision with or without
vertical releasing incisions to reflect a full-thickness
or partial-thickness flap. 11,13 Figure 2 illustrates the CF
technique.
Two independent evaluators collected the data
retrospectively of two patient cohorts from previously
treated PR cases: The experimental group, in which
incisions were performed using the MIF designs, and the
control group, in which the CF approach was employed. For
both groups, a comprehensive review of available clinical
records was conducted regarding the specific incision and Figure 2. Representation of the conventional flap technique performed by
flap techniques employed, the type of membrane and graft a periodontics resident
used, the biological agents utilized, and all post-operative
complications encountered. in data collection: T0, indicating the baseline period
before surgical intervention, and T1, representing the past
At the patient level, demographics captured included follow-up chart, at least 12 months after the procedure.
patient sex and age, while general health data encompassed Intra-operative details specifically focused on the
the presence of diabetes mellitus at the onset of PR dimensions and morphology of the periodontal defects,
therapy and smoking history categorized as non-smoker,
former smoker, or current smoker (along with daily the bone graft used, and the type of membrane used in
cigarette consumption). Each patient’s periodontal status the PR procedure, if any. Any biological agents deployed,
was classified using the staging and grading system antibiotics prescribed, and post-operative complications,
for periodontitis, which includes stage (1–4), grade including infections or membrane exposures, were
(A, B, and C), and extent (localized, generalized), as collected.
32
defined immediately before PR treatment. In addition, For operators, their levels were determined by the year
the analysis considered the duration of each patient’s of the procedure and the corresponding resident level.
follow-up as well as the frequency of maintenance visits R1 was designated as 1 -year residents, R2 as 2 -year
st
nd
after the procedure. residents, and R3 as 3 -year residents.
rd
At the tooth level, tooth-specific clinical parameters,
such as PD, CAL (formerly calculated and recorded in the 2.3. Statistical analysis
chart as the difference between PD and the distance from Statistical analysis was conducted using the Statistical
the free gingival margin to the cementoenamel junction), Package for Social Sciences software (version 22.0, IBM,
BOP, and tooth mobility, were assessed alongside the width United States). The following clinical parameters were
of keratinized tissue. Furcation involvement was examined considered primary outcomes: BOP, PD reduction, CAL
for the molar tooth. Two time points were considered gain, keratinized gingiva (KT) change, GR at T1, and
33
Volume 4 Issue 3 (2025) 98 doi: 10.36922/GTM025080015