Page 238 - EJMO-9-3
P. 238
Eurasian Journal of
Medicine and Oncology ICU pharmacists and clinical outcomes
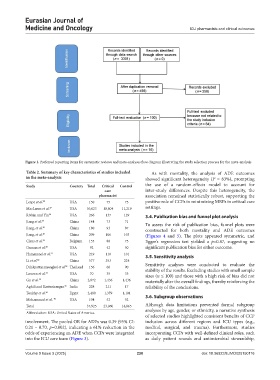
Figure 1. Preferred reporting items for systematic reviews and meta-analyses flow diagram illustrating the study selection process for the meta-analysis
Table 2. Summary of key characteristics of studies included As with mortality, the analysis of ADE outcomes
in the meta‑analysis showed significant heterogeneity (I = 83%), prompting
2
Study Country Total Critical Control the use of a random-effects model to account for
care inter-study differences. Despite this heterogeneity, the
pharmacist association remained statistically robust, supporting the
Leape et al. 25 USA 150 75 75 positive role of CCPs in minimizing MRPs in critical care
MacLaren et al. 37 USA 30,023 18,804 11,219 settings.
Rivkin and Yin 26 USA 266 137 129 3.4. Publication bias and funnel plot analysis
Jiang et al. 27 China 144 73 71 To assess the risk of publication bias, funnel plots were
Jiang, et al. 38 China 180 93 87 constructed for both mortality and ADE outcomes
Jiang, et al. 28 China 209 106 103 (Figures 4 and 5). The plots appeared symmetric, and
Claus et al. 29 Belgium 155 80 75 Egger’s regression test yielded a p=0.87, suggesting no
Oxman et al. 30 USA 92 42 50 significant publication bias for either outcome.
Hammond et al. 31 USA 219 118 101 3.5. Sensitivity analysis
Li et al. 32 China 577 353 224
Dilokpattanamongkol et al. 39 Thailand 156 66 90 Sensitivity analyses were conducted to evaluate the
stability of the results. Excluding studies with small sample
Louzon et al. 33 USA 70 35 35 sizes (n ≤ 100) and those with a high risk of bias did not
Gu et al. 34 China 2,872 1,436 1,436 materially alter the overall findings, thereby reinforcing the
Aghili and Kasturirangan 35 India 228 211 17 reliability of the conclusions.
Toukhy et al. 36 Egypt 2,480 1,379 1,101
Mohammad et al. 40 USA 104 52 52 3.6. Subgroup observations
Total 37,925 23,060 14,865 Although data limitations prevented formal subgroup
Abbreviation: USA: United States of America. analyses by age, gender, or ethnicity, a narrative synthesis
of selected studies highlighted consistent benefits of CCP
involvement. The pooled OR for ADEs was 0.39 (95% CI: inclusion across different regions and ICU types (e.g.,
0.21 – 0.70, p=0.002), indicating a 61% reduction in the medical, surgical, and trauma). Furthermore, studies
odds of experiencing an ADE when CCPs were integrated incorporating CCPs with well-defined clinical roles, such
into the ICU care team (Figure 3). as daily patient rounds and antimicrobial stewardship,
Volume 9 Issue 3 (2025) 230 doi: 10.36922/EJMO025150116