Page 74 - GTM-2-1
P. 74
Global Translational Medicine Mass balance
A B
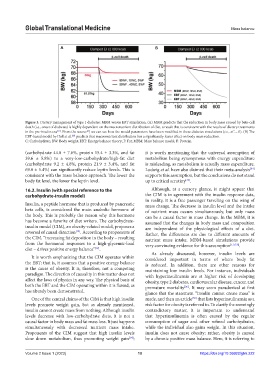
Figure 3. Dietary management of type 1 diabetes: MBM versus EBT simulation. (A) MBM predicts that the reduction in body mass caused by beta-cell
death (i.e., onset of diabetes) is highly dependent on the macronutrient distribution of diet, a result that is consistent with the results of dietary treatments
in the pre-insulin era . From the source , we can see how the model parameters have been modified in these diabetes simulations (i.e., xC = 0). (B) The
[51]
[3]
EBT-based model by Hall et al. predicts that macronutrient distribution has a significantly lesser effect on body mass reduction.
[22]
C: Carbohydrate; BW: Body weight; EBT: Energy balance theory; F: Fat; MBM: Mass balance model; P: Protein.
(carbohydrate 44.0 ± 7.6%, protein 15.4 ± 3.3%, and fat it is worth mentioning that the universal assumption of
39.6 ± 5.8%) to a very-low-carbohydrate/high-fat diet metabolism being synonymous with energy expenditure
(carbohydrate 9.2 ± 4.8%, protein 21.9 ± 3.4%, and fat is misleading, as metabolism is actually mass expenditure.
69.0 ± 5.4%) can significantly reduce leptin levels. This is Ludwig et al. have also claimed that their meta-analysis
[34]
consistent with the mass balance approach. The lower the supports this assumption, but the conclusions do not stand
body fat level, the lower the leptin level. up to critical scrutiny .
[35]
16.2. Insulin (with special reference to the Although, at a cursory glance, it might appear that
carbohydrate-insulin model) the CIM is in agreement with the insulin response data,
in reality, it is a free passenger traveling on the wing of
Insulin, a peptide hormone that is produced by pancreatic mass change. The decrease in insulin level and the intake
beta cells, is considered the main anabolic hormone of of nutrient mass occurs simultaneously, but only mass
the body. This is probably the reason why this hormone can be a causal factor in mass change. In the MBM, it is
has become a favorite of diet writers. The carbohydrate- assumed that the changes in body mass and composition
insulin model (CIM), an obesity-related model, proposes a are independent of the physiological effects of a diet.
reversal of causal direction . According to proponents of Rather, the differences are due to different amounts of
[14]
the CIM, “increasing fat deposition in the body – resulting nutrient mass intake. MBM-based simulations provide
from the hormonal responses to a high-glycemic-load very convincing evidence for this assumption [1,3,7,8] .
diet – drives positive energy balance” .
[14]
As already discussed, however, insulin levels are
It is worth emphasizing that the CIM operates within considered important in terms of where body fat
the EBT; that is, it assumes that a positive energy balance is reduced. In addition, there are other reasons for
is the cause of obesity. It is, therefore, not a competing maintaining low insulin levels. For instance, individuals
paradigm. The direction of causality in this matter does not with hyperinsulinemia are at higher risk of developing
affect the laws of physics in any way. The physical basis of obesity, type 2 diabetes, cardiovascular disease, cancer, and
both the EBT and the CIM operating within it is flawed, as premature mortality . It may seem paradoxical at first
[36]
has already been demonstrated. glance that the statement “insulin cannot create mass” is
One of the central claims of the CIM is that high insulin made, and then an article that lists hyperinsulinemia as a
[36]
levels promote weight gain, but as already mentioned, risk factor for obesity is referred to. To clarify the seemingly
insulin cannot create mass from nothing. Although insulin contradictory matter, it is important to understand
levels decrease with low-carbohydrate diets, it is not a that hyperinsulinemia is often caused by the regular
causal factor in body mass and fat mass loss. It just happens consumption of sugar and other refined carbohydrates,
simultaneously with decreased nutrient mass intake. while the individual also gains weight. In this situation,
Proponents of the CIM suggest that high insulin levels insulin does not cause obesity; rather, obesity is caused
slow down metabolism, thus promoting weight gain ; by a chronic positive mass balance. Here, it is referring to
[14]
Volume 2 Issue 1 (2023) 10 https://doi.org/10.36922/gtm.222