Page 244 - IJB-9-1
P. 244
International Journal of Bioprinting 3D printing of smart constructs for precise medicine
A B
C
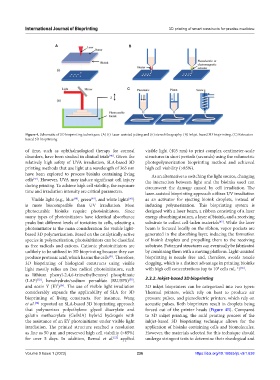
Figure 4. Schematic of 3D bioprinting techniques. (A) (i) Laser-assisted jetting and (ii) stereolithography. (B) Inkjet-based 3D bioprinting. (C) Extrusion-
based 3D bioprinting.
of time, such as ophthalmological therapy for corneal visible light (405 nm) to print complex centimeter-scale
disorders, have been studied in clinical trials . Given the structures in short periods (seconds) using the volumetric
[46]
relatively high safety of UVA irradiation, SLA-based 3D photopolymerization bioprinting method and achieved
printing methods that use light at a wavelength of 365 nm high cell viability (>85%).
have been explored to process bioinks containing living As an alternative to switching the light source, changing
cells . However, UVA may induce significant cell injury the interaction between light and the bioinks used can
[47]
during printing. To achieve high cell viability, the exposure circumvent the damage caused by cell irradiation. The
time and irradiation intensity are critical parameters. laser-assisted bioprinting approach utilizes UV irradiation
Visible light (e.g., blue , green , and white lights ) as an activator for ejecting bioink droplets, instead of
[48]
[49]
[50]
is more biocompatible than UV irradiation. Most inducing polymerization. This bioprinting system is
photocurable bioinks require photoinitiators. Since designed with a laser beam, a ribbon consisting of a laser
many types of photoinitiators have identical absorbance energy absorbing stratum, a layer of bioink, and a receiving
peaks but different levels of toxicities to cells, selecting a substrate to collect cell-laden materials . While the laser
[45]
photoinitiator is the main consideration for visible light- beam is focused locally on the ribbon, vapor pockets are
based 3D polymerization. Based on the catalytically active generated in the absorbing layer, inducing the formation
species in polymerization, photoinitiators can be classified of bioink droplets and propelling them to the receiving
as free radicals and cations. Cationic photoinitiators are substrate. Patterned structures can eventually be fabricated
unlikely to be utilized in 3D bioprinting because they can by combining them with a moving platform. Light-assisted
produce protonic acid, which harms the cells . Therefore, bioprinting is nozzle free and, therefore, avoids nozzle
[51]
3D bioprinting of biological constructs using visible clogging, which is a distinct advantage in printing bioinks
light mostly relies on free radical photoinitiators, such with high cell concentrations (up to 10 cells mL ) .
8
−1 [56]
as lithium phenyl-2,4,6-trimethylbenzoyl phosphinate
[52]
[53]
(LAP) , hexahydrate/sodium persulfate (RU/SPS) , 2.3.2. Inkjet-based 3D bioprinting
and eosin Y (EY) . The use of visible light irradiation 3D inkjet bioprinters can be categorized into two types:
[54]
considerably expands the applicability of SLA for 3D Thermal printers, which rely on heat to produce air
bioprinting of living constructs. For instance, Wang pressure pulses, and piezoelectric printers, which rely on
et al. reported an SLA-based 3D bioprinting approach acoustic pulses. Both bioprinters result in droplets being
[54]
that polymerizes polyethylene glycol diacrylate and forced out of the printer heads (Figure 4B). Compared
gelatin methacrylate (GelMA) hybrid hydrogels with to 3D inkjet printing, the mild printing process of the
the assistance of an EY photoinitiator under visible light inkjet-based 3D bioprinting technique allows for the
irradiation. The printed structure reached a resolution application of bioinks containing cells and biomolecules.
as fine as 50 μm and preserved high cell viability (>85%) However, the materials selected for this technique should
for over 5 days. In addition, Bernal et al. applied undergo stringent tests to determine their rheological and
[55]
Volume 9 Issue 1 (2023) 236 https://doi.org/10.18063/ijb.v9i1.638