Page 46 - TD-3-2
P. 46
Tumor Discovery PG of maxillary median gingiva in a pediatric patient
A B C
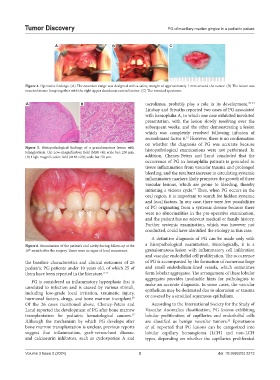
Figure 4. Operative findings. (A) The resection range was designed with a safety margin of approximately 1 mm around the tumor. (B) The lesion was
resected in one lump together with the right upper deciduous central incisor. (C) The resected specimen.
A B tacrolimus, probably play a role in its development. 29-34
Lindsay and Srivaths reported two cases of PG associated
with hemophilia A, in which one case exhibited involuted
presentation, with the lesion slowly resolving over the
subsequent weeks, and the other demonstrating a lesion
which was completely resolved following infusion of
recombinant factor 8. However, there is no confirmation
13
on whether the diagnosis of PG was accurate because
Figure 5. Histopathological findings of a granulomatous lesion with histopathological examinations were not performed. In
telangiectasia. (A) Low-magnification field (MM ×4); scale bar: 250 μm.
(B) High-magnification field (MM ×20); scale bar: 50 μm. addition, Cheney-Peters and Lund concluded that the
occurrence of PG in hemophilia patients is grounded in
tissue inflammation from vascular trauma and prolonged
bleeding, and the resultant increase in circulating systemic
inflammatory markers likely promotes the growth of these
vascular lesions, which are prone to bleeding, thereby
initiating a vicious cycle. Thus, when PG occurs in the
17
oral region, it is important to search for hidden systemic
and local factors. In our case, there were few possibilities
of PG originating from a systemic disease because there
were no abnormalities in the pre-operative examination,
and the patient has no relevant medical or family history.
Further systemic examination, which was however not
conducted, could have identified the etiology in this case.
A definitive diagnosis of PG can be made only with
Figure 6. Examination of the patient’s oral cavity during follow-up at the a histopathological examination. Histologically, it is a
18 month after the surgery. There were no signs of local recurrence. granulomatous lesion with inflammatory cell infiltration
th
and vascular endothelial cell proliferation. The occurrence
the baseline characteristics and clinical outcomes of 26 of PG is accompanied by the formation of numerous large
pediatric PG patients under 10 years old, of which 25 of and small endothelium-lined vessels, which sometimes
them have been reported in the literature. 4-27 form lobular aggregates. The arrangement of these lobular
aggregates provides invaluable hints for pathologists to
PG is considered an inflammatory hyperplasia that is
unrelated to infection and is caused by various stimuli, make an accurate diagnosis. In some cases, the vascular
epithelium may be decimated due to ulceration or trauma
including low-grade local irritation, traumatic injury, or covered by a stratified squamous epithelium.
hormonal factors, drugs, and bone marrow transplant.
28
Of the 26 cases mentioned above, Cheney-Peters and According to the International Society for the Study of
Lund reported the development of PG after bone marrow Vascular Anomalies classification, PG lesions exhibiting
transplantation for pediatric hematological cancers. lobular proliferation of capillaries and endothelial cells
17
Although the mechanism by which PG develops after are classified as benign vascular tumors. Epivatianos
35
bone marrow transplantation is unclear, previous reports et al. reported that PG lesions can be categorized into
suggest that inflammation, graft-versus-host disease, lobular capillary hemangioma (LCH) and non-LCH
and calcineurin inhibitors, such as cyclosporine A and types, depending on whether the capillaries proliferated
Volume 3 Issue 2 (2024) 3 doi: 10.36922/td.2213