Page 43 - ARNM-2-4
P. 43
Advances in Radiotherapy
& Nuclear Medicine Outcomes of durations in 2D and 3D BT for CCA
IVA of the disease, respectively. The inclusion criteria stage, and pathology, with a matching tolerance of 0.02.
were patients clinically diagnosed with cervical cancer, Matching was conducted separately for the overall dataset,
including squamous cell carcinoma, adenocarcinoma, patients who received 2D brachytherapy, and patients who
adenosquamous carcinoma, or small cell carcinoma, with received 3D brachytherapy. From the overall dataset of
clinical staging ranging from IB to IVA. Furthermore, data 649 patients, PSM yielded 162 pairs (total, 324 patients’
were stratified according to planned external radiation data). From the subset of 525 patients who received 2D
dose, FIGO staging, radiation therapy technique, and brachytherapy, PSM yielded 88 pairs (total, 176 patients’
whether concurrent chemotherapy was administered. The data). From the subset of 124 patients who received 3D
results were summarized and tabulated (Table 1). brachytherapy, PSM yielded 25 pairs (total, 50 patients’
data). The differences and characteristic data before and
2.2. Propensity score matching (PSM) after PSM are shown in Table 2.
The data of the 649 patients with cervical cancer were
classified and analyzed. Based on whether the treatment 2.3. Inverse probability of treatment weighting
duration exceeded 56 days or not, the patients were (IPTW)
divided into the OG (>56 days) or CG (≤56 days). PSM Further statistical analysis was performed using the IPTW
was performed using factors such as age group, FIGO method. The confounding factors encompassed age group,
FIGO stage, pathology, chemotherapy, and brachytherapy.
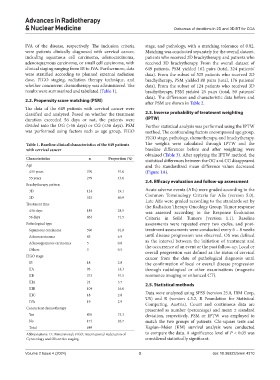
Table 1. Baseline clinical characteristics of the 649 patients The weights were calculated through IPTW and the
with cervical cancer baseline differences before and after weighting were
obtained (Table 3). After applying the IPTW method, the
Characteristics n Proportion (%) statistical differences between the OG and CG disappeared
Age and the standardized mean difference values decreased
≤55 years 370 57.0 (Figure 1A).
55 years 279 43.0
Brachytherapy pattern 2.4. Efficacy evaluation and follow-up assessment
3D 124 19.1 Acute adverse events (AEs) were graded according to the
2D 525 80.9 Common Terminology Criteria for AEs (version 5.0).
Late AEs were graded according to the standards set by
Treatment time the Radiation Therapy Oncology Group. Tumor response
≤56 days 185 28.5 was assessed according to the Response Evaluation
56 days 464 71.5 Criteria in Solid Tumors (version 1.1). Baseline
Pathological type assessments were repeated every two cycles, and post-
Squamous carcinoma 596 91.8 treatment assessments were conducted every 6 – 8 weeks
Adenocarcinoma 45 6.9 until disease progression was observed. OS was defined
as the interval between the initiation of treatment and
Adenosquamous carcinoma 5 0.8
Others 3 0.5 the occurrence of an event or the past follow-up. Local or
overall progression was defined as the status of cervical
FIGO stage cancer from the date of pathological diagnosis until
IB 18 2.8 the confirmation of local or overall disease progression
IIA 93 14.3 through radiological or other examinations (magnetic
IIB 373 57.5 resonance imaging or enhanced CT).
IIIA 24 3.7
2.5. Statistical methods
IIIB 104 16.0
IIIC 18 2.8 Data were analyzed using SPSS (version 25.0, IBM Corp,
US) and R (version 4.3.2, R Foundation for Statistical
IVA 19 2.9 Computing, Austria). Count and continuous data are
Concurrent chemotherapy presented as number (percentage) and mean ± standard
Yes 476 73.3 deviation, respectively. PSM or IPTW was employed to
No 173 26.7 match the two groups of patients. Chi-square tests and
Total 649 Kaplan–Meier (KM) survival analysis were conducted
Abbreviations: D: Dimensional; FIGO: International Federation of to compare the data. A significance level of P < 0.05 was
Gynecology and Obstetrics staging. considered statistically significant.
Volume 2 Issue 4 (2024) 3 doi: 10.36922/arnm.4310