Page 15 - JCTR-11-3
P. 15
Journal of Clinical and
Translational Research Lateral patellar instability in deep flexion
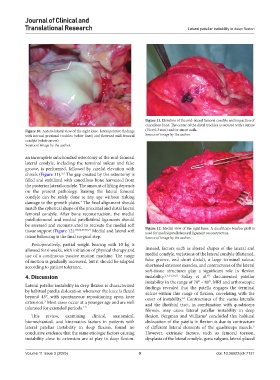
Figure 11. Elevation of the mid-lateral femoral condyle and impaction of
cancellous bone. The center of the distal trochlea is secured with a suture
Figure 10. Antero-lateral view of the right knee. Intraoperative findings (Vicryl, 5 mm) and/or smart nails.
with normal proximal trochlea (white lines) and flattened mid-femoral Source of image by the author.
condyle (white arrow).
Source of image by the author.
an incomplete subchondral osteotomy of the mid-femoral
lateral condyle, including the terminal sulcus and false
groove, is performed, followed by careful elevation with
chisels (Figure 11). The gap created by the osteotomy is
2,4
filled and stabilized with cancellous bone harvested from
the posterior lateral condyle. The amount of lifting depends
on the present pathology. Raising the lateral femoral
condyle can be safely done at any age without risking
damage to the growth plates. The final alignment should
4
match the spherical shape of the proximal and distal lateral
femoral condyle. After bone reconstruction, the medial
patellofemoral and medial patellotibial ligaments should
be assessed and reconstructed to recreate the medial soft
tissue support (Figure 12). 33,36,37,70,71 Medial and lateral soft Figure 12. Medial view of the right knee. A quadriceps tendon graft is
used for medial patellofemoral ligament reconstruction.
tissue balancing is the final surgical step. Source of image by the author.
Postoperatively, partial weight bearing with 10 kg is
allowed for 6 weeks, with initiation of physical therapy and Instead, factors such as altered shapes of the lateral and
use of a continuous passive motion machine. The range medial condyle, variations of the lateral condyle (flattened,
of motion is gradually increased, but it should be adapted false groove, and short distal), a large terminal sulcus,
according to patient tolerance. shortened extensor muscles, and contractures of the lateral
soft-tissue structures play a significant role in flexion
4. Discussion instability. 2-5,15,25,63 Sallay et al. documented patellar
63
instability in the range of 70° – 80°. MRI and arthroscopic
Lateral patellar instability in deep flexion is characterized findings revealed that the patella engages the terminal
by habitual patella dislocation whenever the knee is flexed sulcus within this range of flexion, correlating with the
beyond 45°, with spontaneous repositioning upon knee onset of instability. Contractures of the vastus lateralis
63
extension. Most cases occur at a younger age and are well and the iliotibial tract, in combination with quadriceps
3
tolerated for extended periods. 3-5 fibrosis, may cause lateral patellar instability in deep
This review, examining clinical, anatomical, flexion. Bergman and Williams concluded that habitual
5
biomechanical, and kinematics factors in patients with dislocation of the patella in flexion is due to contracture
lateral patellar instability in deep flexion, found no of different lateral elements of the quadriceps muscle.
5
conclusive evidence that the same etiologic factors causing However, extrinsic factors, such as femoral torsion,
instability close to extension are at play in deep flexion. dysplasia of the lateral condyle, genu valgum, lateral placed
Volume 11 Issue 3 (2025) 9 doi: 10.36922/jctr.7131