Page 62 - JCTR-9-4
P. 62
278 Li et al. | Journal of Clinical and Translational Research 2023; 9(4): 272-281
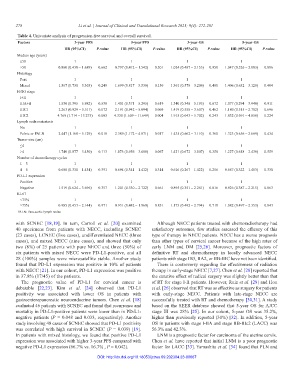
Table 4. Univariate analysis of progression-free survival and overall survival.
Factors 3‑year PFS 5‑year PFS 3‑year OS 5‑year OS
HR (95%CI) P‑value HR (95%CI) P‑value HR (95%CI) P‑value HR (95%CI) P‑value
Median age (years)
≤50 1 1 1 1
>50 0.860 (0.438 – 1.689) 0.662 0.797 (0.412 – 1.542) 0.501 1.024 (0.487 – 2.153) 0.950 1.047 (0.526 – 2.083) 0.896
Histology
Pure 1 1 1 1
Mixed 1.567 (0.730 – 3.363) 0.249 1.699 (0.817 – 3.530) 0.156 1.361 (0.578 – 3.206) 0.480 1.406 (0.632 – 3.128) 0.404
FIGO stage
I+II 1 1 1 1
IIIA+B 1.530 (0.395 – 5.982) 0.538 1.401 (0.371 – 5.295) 0.619 1.340 (0.346 – 5.195) 0.672 1.077 (0.294 – 3.940) 0.911
IIIC1 2.263 (0.929 – 5.511) 0.072 2.191 (0.942 – 5.094) 0.069 1.419 (0.558 – 3.607) 0.462 1.180 (0.515 – 2.702) 0.696
IIIC2 4.769 (1.714 – 13.275) 0.003 4.330 (1.609 – 11.649) 0.004 1.915 (0.643 – 5.702) 0.243 1.832 (0.691 – 4.858) 0.224
Lymph node metastasis
No 1 1 1 1
Pelvic or PALN 2.447 (1.168 – 5.129) 0.018 2.389 (1.172 – 4.871) 0.017 1.435 (0.662 – 3.110) 0.360 1.323 (0.656 – 2.669) 0.434
Tumor size (cm)
≤4 1 1 1 1
>4 1.740 (0.877 – 3.450) 0.113 1.873 (0.956 – 3.668) 0.067 1.421 (0.672 – 3.007) 0.358 1.227 (0.618 – 2.439) 0.559
Number of chemotherapy cycles
1 – 3 1 1 1 1
4 – 6 0.688 (0.331 – 1.434) 0.391 0.694 (0.341 – 1.412) 0.314 0.616 (0.267 – 1.422) 0.256 0.687 (0.322 – 1.463) 0.330
PD-L1 expression
Positive 1 1 1 1
Negative 1.519 (0.624 – 3.696) 0.357 1.201 (0.530 – 2.722) 0.661 0.895 (0.351 – 2.281) 0.816 0.926 (0.387 – 2.215) 0.863
Ki-67
<75% 1 1 1 1
≥75% 0.985 (0.453 – 2.144) 0.971 0.931 (0.442 – 1.960) 0.851 1.173 (0.492 – 2.794) 0.718 1.082 (0.497 – 2.353) 0.843
PALN: Para-aortic lymph nodes
with SCNEC [18,19]. In turn, Carroll et al. [20] examined Although NECC patients treated with chemoradiotherapy had
40 specimens from patients with NECC, including SCNEC satisfactory outcomes, few studies assessed the efficacy of this
(23 cases), LCNEC (five cases), undifferentiated NECC (three type of therapy in NECC patients. NECC has a worse prognosis
cases), and mixed NECC (nine cases), and showed that only than other types of cervical cancer because of the high rates of
two (8%) of 25 patients with pure NECC and three (50%) of early LNM and DM [25,26]. Moreover, prognostic factors of
six patients with mixed NECC were PD-L1-positive, and all definitive RT and chemotherapy in locally advanced NECC
28 (100%) samples were microsatellite stable. Another study patients with stage IB3, IIA2, or IIB-IIIC have not been identified.
found that PD-L1 expression was positive in 10% of patients There is controversy regarding the effectiveness of radiation
with NECC [21]. In our cohort, PD-L1 expression was positive therapy in early-stage NECC [7,27]. Chen et al. [28] reported that
in 37.8% (17/45) of the patients. the curative effect of radical surgery was slightly better than that
The prognostic value of PD-L1 for cervical cancer is of RT for stage I-II patients. However, Ruiz et al. [29] and Hou
debatable [22,23]. Kim et al. [24] observed that PD-L1 et al. [26] observed that RT was as effective as surgery for patients
positivity was associated with lower OS in patients with with early-stage NECC. Patients with late-stage NECC are
gastroenteropancreatic neuroendocrine tumors. Chen et al. [18] successfully treated with RT and chemotherapy [30,31]. A study
evaluated 46 patients with SCNEC and found that recurrence and based on the SEER database showed that 5-year OS for AJCC
mortality in PD-L1-positive patients were lower than in PD-L1- stage III was 28% [25]. In our cohort, 5-year OS was 35.2%,
negative patients (P = 0.048 and 0.033, respectively). Another higher than previously reported (30%) [32]. In addition, 5-year
study involving 48 cases of SCNEC showed that PD-L1 positivity OS in patients with stage I-IIA and stage IIB-IIIc2 (LACC) was
was correlated with high survival in SCNEC (P = 0.039) [19]. 56.3% and 42.3%.
In patients with mixed histology, we found that positive PD-L1 LNM is a prognostic factor for carcinoma of the uterine cervix.
expression was associated with higher 3-year PFS compared with Chen et al. have reported that initial LNM is a poor prognostic
negative PD-L1 expression (66.7% vs. 16.7% , P = 0.042). factor for LACC [33]. Yamashita et al. [34] found that PLN and
DOI: http://dx.doi.org/10.18053/jctres.09.202304.23-00067