Page 46 - GTM-1-2
P. 46
Global Translational Medicine Cirrhosis and hepatocellular carcinoma
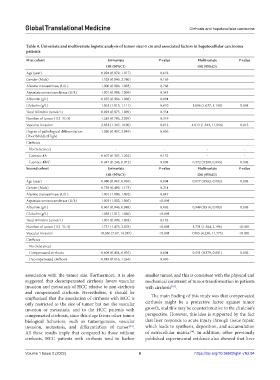
Table 4. Univariate and multivariate logistic analysis of tumor size>5 cm and associated factors in hepatocellular carcinoma
patients
First cohort Univariate P‑value Multivariate P‑value
OR (95%CI) OR (95%CI)
Age (year) 0.994 (0.972, 1.017) 0.618
Gender (Male) 1.528 (0.840, 2.780) 0.165
Alanine transaminase (U/L) 1.000 (0.996, 1.003) 0.768
Aspartate aminotransferase (U/L) 1.001 (0.998, 1.004) 0.543
Albumin (g/L) 0.955 (0.906, 1.008) 0.094
Globulin (g/L) 1.062 (1.015, 1.111) 0.010 1.096 (1.037, 1.158) 0.001
Total Bilirubin (umol/L) 0.992 (0.975, 1.009) 0.354
Number of tumor (1/2–3/>3) 1.283 (0.786, 2.095) 0.319
Vascular invasion 3.832 (1.347, 10.90) 0.012 4.013 (1.342, 11.996) 0.013
Degree of pathological differentiation 1.096 (0.407, 2.949) 0.856
(Poor/Middle/High)
Cirrhosis
No (reference) - - - -
Laennec 4A 0.607 (0.307, 1.202) 0.152 - -
Laennec 4B/C 0.447 (0.246, 0.812) 0.008 0.372 (0.200, 0.693) 0.002
Second cohort Univariate P‑value Multivariate P‑value
OR (95%CI) OR (95%CI)
Age (year) 0.980 (0.967, 0.994) 0.004 0.977 (0.962, 0.992) 0.003
Gender (Male) 0.758 (0.490, 1.173) 0.214
Alanine transaminase (U/L) 1.001 (1.000, 1.002) 0.047
Aspartate aminotransferase (U/L) 1.003 (1.002, 1.005) <0.001
Albumin (g/L) 0.967 (0.946, 0.988) 0.002 0.949 (0.916, 0.983) 0.003
Globulin (g/L) 1.038 (1.017, 1.060) <0.001
Total Bilirubin (umol/L) 1.001 (0.999, 1.003) 0.192
Number of tumor (1/2–3/>3) 1.751 (1.475, 2.078) <0.001 1.731 (1.364, 2.196) <0.001
Vascular invasion 10.056 (7.07, 14.287) <0.001 7.065 (4.238, 11.775) <0.001
Cirrhosis
No (reference) - - - -
Compensated cirrhosis 0.609 (0.434, 0.855) 0.004 0.551 (0.379, 0.801) 0.002
Decompensated cirrhosis 0.883 (0.616, 1.264) 0.496
association with the tumor size. Furthermore, it is also smaller tumor, and this is consistent with the physical and
suggested that decompensated cirrhosis favors vascular mechanical constraint of tumor transformation in patients
invasion and metastasis of HCC relative to non-cirrhosis with cirrhosis .
[10]
and compensated cirrhosis. Nevertheless, it should be
emphasized that the association of cirrhosis with HCC is The main finding of this study was that compensated
only restricted to the size of tumor but not the vascular cirrhosis might be a protective factor against tumor
invasion or metastasis, and to the HCC patients with growth, and this may be counterintuitive to the clinician’s
compensated cirrhosis, since this stage favors other tumor perspective. However, this idea is supported by the fact
biological behaviors, such as tumorigenesis, vascular that liver responds to acute injury through tissue repair,
invasion, metastasis, and differentiation of tumor . which leads to synthesis, deposition, and accumulation
[13]
[14]
All these results imply that compared to those without of extracellular matrix . In addition, other previously
cirrhosis, HCC patients with cirrhosis tend to harbor published experimental evidence also showed that liver
Volume 1 Issue 2 (2022) 6 https://doi.org/10.36922/gtm.v1i2.94