Page 125 - GTM-4-1
P. 125
Global Translational Medicine AA amyloidosis in rheumatoid arthritis
Table 4. (Continued)
f/m GI-Tract AA amyloidosis Avg Cause of death Cl+/Cl-
a A I ret VV AA V BM Myo v n giAAa/Pt
SD 0.97 0.78 0.93 0.89 0.83 0.56 0.76 0.55 0.57 0.33 0.34 0.51 – –
“0” n 2 2 7 11 12 12 18 16 23 24 25 2 – –
“+” n 29 29 24 20 19 19 13 15 8 7 6 29 – –
Prev. % 93.548 93.548 77.419 64.516 61.290 61.290 41.935 48.387 25.806 22.581 19.355 93.548 – –
Sev. % 70.796 47.022 40.323 25.720 23.280 17.548 16.839 12.086 9.688 5.011 4.290 24.782 – –
Notes: (i) Table 4 is organized based on the increasing values of average AA deposits per patient (vertical columns) and the distribution of AA deposits
across gastrointestinal (GI) tissue structures arranged in order of severity (horizontal rows).
(ii) Sporadic vasculitis associated with carcinoma (CA).
a
(iii) Definition: Pr. n /y: Protocol number/year; Prevalence/patient in % (Prev. %): positive (“+”) cases in % of “count”; Severity in % (Sev. %): “Avg”
0]
in % of maximum “3” value of severity; CoD: Cause of death; Cl+: Clinically recognized; Cl-: Clinically not recognized; f: female; m: male;
NA: Tissue blocks of GI tract were not available; ND: No data; SD: Standard deviation; “–”: Died of other causes or were not diagnosed clinically;
Avg: Average; rAAa-U: Uremia due to massive AA deposition in the kidneys (rAAa) with consecutive renal insufficiency (n=17); cAAa: Lethal
outcome exclusively caused by cardiac amyloidosis (n=3) (322/81, 430/80, 45/74); in additional 5 (243/87, 287/91, 395/76, 245/88, 367/75) of 31
patients, cardiac amyloidosis contributed to the death; a: Arteriole; A: Small artery; AA: Medium size artery; v: Venule; V: Small vein; VV: Medium
size vein; I: Interstitial collagen fiber; ret: Reticulin fiber (collagen III); BM: Basement membrane of intestinal gland; Myo: Smooth muscle cells of
tunica muscularis; n: Nerve.
(iv) In 2 (6.45%) of 31 rheumatoid arthritis patients with sAAa, no AA deposition was detected in the GI tract, representing a latent stage of GI
amyloidosis (AA deposits=0.00).
(v) In 17 (54.84%) of 31 patients with mild GI amyloidosis, the AA deposit level was <0,8, classifying them as mild.
(vi) In 12 (38.71%) of 31 patients, the GI AA deposit level was >0.8, which was considered severe.
(vii) sAAa was the cause of death in 23 of 31 patients with GI AA amyloidosis (giAAa); 8 of these 23 cases were clinically diagnosed.
(viii) While GI amyloidosis itself was not a direct cause of mortality, three of the four patients with the most severe giAAa also had the most severe
renal amyloidosis. These patients (255/83, 101/90, 265/80, and 53/87) represented the pre-mortem stage of fatal uremia.
Abbreviations: AA: Amyloid A; giAAa: GI AA Amyloidosis.
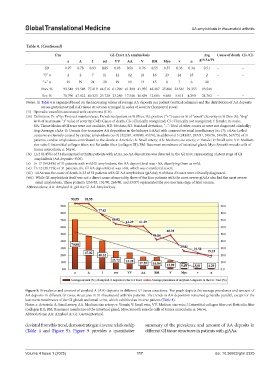
Figure 9. Prevalence and amount of amyloid A (AA) deposits in different GI tissue structures. The graph depicts the average prevalence and amount of
AA deposits in different GI tissue structures in 31 rheumatoid arthritis patients. The trends in AA deposition remained generally parallel, except for the
basement membranes of the GI glands and small veins, which exhibited an inverse pattern (Table 4).
Notes: a: Arteriole; A: Small artery; AA: Medium size artery; v: Venule; V: Small vein; VV: Medium size vein; I: Interstitial collagen fiber; ret: Reticulin fiber
(collagen III); BM: Basement membrane of the intestinal gland; Myo: Smooth muscle cells of tunica muscularis; n: Nerve.
Abbreviations: AA: Amyloid A; GI: Gastrointestinal.
deviated from this trend, demonstrating an inverse relationship summary of the prevalence and amount of AA deposits in
(Table 4 and Figure 9). Figure 9 provides a quantitative different GI tissue structures in patients with giAAa.
Volume 4 Issue 1 (2025) 117 doi: 10.36922/gtm.5325