Page 49 - GTM-4-3
P. 49
Global Translational Medicine Evolution of tunneling techniques
A B C
D E F
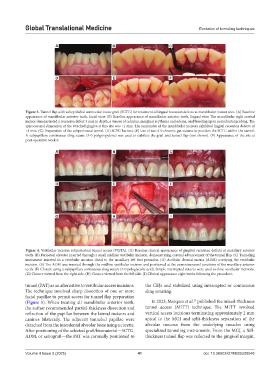
Figure 3. Tunnel flap with subepithelial connective tissue graft (SCTG) for treatment of lingual recession defects at mandibular incisor sites. (A) Baseline
appearance of mandibular anterior teeth, facial view. (B) Baseline appearance of mandibular anterior teeth, lingual view. The mandibular right central
incisor demonstrated a recession defect 3 mm in depth, a veneer of calculus, marginal erythema and edema, and bleeding upon periodontal probing. The
apicocoronal dimension of the attached gingiva at this site was <1 mm. The remainder of the mandibular incisors exhibited lingual recession defects of
<1 mm. (C) Preparation of the subperiosteal tunnel. (D) SCTG harvest. (E) Use of two 4-0 chromic gut sutures to position the SCTG within the tunnel.
A subpapillary continuous sling suture (5-0 polypropylene) was used to stabilize the graft and tunnel flap (not shown). (F) Appearance of the site at
post-operative week 6.
A B C
D E F
G H I
Figure 4. Vestibular incision subperiosteal tunnel access (VISTA). (A) Baseline clinical appearance of gingival recession defects at maxillary anterior
teeth. (B) Periosteal elevator inserted through a small midline vestibular incision, demonstrating coronal advancement of the tunnel flap. (C) Tunneling
instrument inserted in a vestibular incision distal to the maxillary left first premolar. (D) Acellular dermal matrix (ADM) overlying the vestibular
incision. (E) The ADM was inserted through the midline vestibular incision and positioned at the cementoenamel junctions of the maxillary anterior
teeth. (F) Closure using a subpapillary continuous sling suture (7-0 polyglycolic acid). Simple interrupted sutures were used to close vestibular incisions.
(G) Closure viewed from the right side. (H) Closure viewed from the left side. (I) Clinical appearance eight weeks following the procedure.
tunnel (PAT) as an alternative to vestibular access incisions. the CEJs and stabilized using interrupted or continuous
The technique involved sharp dissection of one or more sling suturing.
facial papillae to permit access for tunnel flap preparation
13
(Figure 5). When treating all mandibular anterior teeth, In 2023, Marques et al. published the mixed-thickness
the author recommended partial-thickness dissection and tunnel access (MiTT) technique. The MiTT involved
reflection of the papillae between the lateral incisors and vertical access incisions terminating approximately 2 mm
canines bilaterally. The adjacent tunneled papillae were apical to the MGJ and split-thickness separation of the
detached from the interdental alveolar bone using a curette. alveolar mucosa from the underlying muscles using
After positioning of the selected graft/biomaterial—SCTG, specialized tunneling instruments. From the MGJ, a full-
ADM, or xenograft—the PAT was coronally positioned to thickness tunnel flap was reflected to the gingival margin,
Volume 4 Issue 3 (2025) 41 doi: 10.36922/GTM025220048