Page 295 - IJB-9-3
P. 295
International Journal of Bioprinting 3D bioprinting as a prospective therapeutic strategy for LSCD
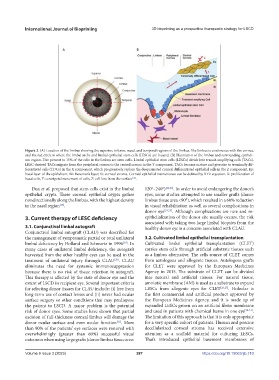
Figure 2. (A) Location of the limbus showing the superior, inferior, nasal, and temporal regions of the limbus. The limbus is continuous with the cornea,
and the red circle is where the limbal niche and limbal epithelial stem cells (LESCs) are located. (B) Illustration of the limbus and surrounding epitheli-
um region. Five percent to 15% of the cells in the limbus are stem cells. Limbal epithelial stem cells (LESCs) divide into transit-amplifying cells (TACs).
LESC-derived TACs migrate from the peripheral cornea to the central cornea in the Y component. TACs become mature and give rise to terminally dif-
ferentiated cells (TDCs) in the X component, which progressively replace the desquamated corneal differentiated epithelial cells in the Z component. Ep:
basal layer of the epithelium; BL: Bowman’s layer; St: corneal stroma. Corneal epithelial maintenance can be defined by XYZ equation. X: proliferation of
basal cells, Y: centripetal movement of cells, Z: cell loss from the surface .
[14]
Dua et al. proposed that stem cells exist in the limbal 120°–240°) [22,23] . In order to avoid endangering the donor’s
epithelial crypts. These corneal epithelial crypts gather eyes, some studies attempted to use smaller grafts (donor
nondirectionally along the limbus, with the highest density limbus tissue area <90°), which resulted in a 60% reduction
[18]
in the nasal region . in visual rehabilitation as well as several complications in
donor eye [24,25] . Although complications are rare and re-
3. Current therapy of LESC deficiency epithelialization of the donor site usually occurs, the risk
associated with taking two large limbal biopsies from the
3.1. Conjunctival limbal autograft healthy donor eye is a concern associated with CLAU.
Conjunctival limbal autograft (CLAU) was described for
the management of symptomatic partial or total unilateral 3.2. Cultivated limbal epithelial transplantation
limbal deficiency by Holland and Schwartz in 1996 . In Cultivated limbal epithelial transplantation (CLET)
[19]
many cases of unilateral limbal deficiency, the autograft carries stem cells through artificial substrate tissues such
harvested from the other healthy eyes can be used in the as a limbus alternative. The cells source of CLET comes
treatment of unilateral injury through CLAU . CLAU from autologous and allogenic tissues. Autologous grafts
[20]
eliminates the need for systemic immunosuppression for CLET were approved by the European Medicines
because there is no risk of tissue rejection in autograft. Agency in 2015. The substrate of CLET can be divided
This therapy is affected by the state of donor eye and the into natural and artificial tissues. For natural tissue,
extent of LSCD in recipient eye. Several important criteria amniotic membrane (AM) is used as a substrate to expand
for selecting donor tissues for CLAU include: (i) free from LESCs from allogenic eyes for CLET [26,27] . Holoclar is
long-term use of contact lenses and (ii) never had ocular the first commercial and artificial product approved by
surface surgery or other conditions that may predispose the European Medicines Agency, and it is made up of
the patient to LSCD. A major problem is the potential expanded LESCs grown on an artificial fibrin membrane
risk of donor eyes. Some studies have shown that partial and used in patients with chemical burns in one eye [28-31] .
excision of full-thickness corneal limbus will damage the The limitation of this approach is that it is only appropriate
donor ocular surface and even ocular function . More for a very specific cohort of patients. Human and porcine
[21]
than 90% of the patients’ eye surfaces were restored with decellularized corneal stroma has received extensive
overwhelmingly (greater than 80%) successful visual attention as a scaffold material for culturing LESCs.
outcomes when using large grafts (donor limbus tissue area: Thai’s introduced epithelial basement membranes of
Volume 9 Issue 3 (2023) 287 https://doi.org/10.18063/ijb.710